- SELF STUDY MODULES
- 1. Intro to TBI
- 2. Communication
- 3. Skills for independence
- 4. Cognitive changes
- 5. Behaviour changes
- 6. Sexuality
- 7. Case management (BIR)
- 8. No longer available
- 9. Mobility & motor control
- 10. Mental health & TBI:
an introduction - 11. Mental health problems
and TBI: diagnosis
& management - 12. Working with Families
after Traumatic Injury:
An Introduction - 13. Goal setting
- 13.0 Aims
- 13.0A Take the PRE-Test
- PART A:
SETTING GOALS
IN REHABILITATION
- PART B: TEAMS &
GOALS - 13.B1 Collaborative goal setting
- 13.B2 Rehabilitation teams & goals
- 13.B3 Quality & Evaluation checklists
- 13.B4 Take home messages
- PART C: WORKSHEETS
- 13.C1 SMARTAAR
Goals Worksheet A - 13.C2 SMARTAAR
Goals Worksheet B - 13.C3 Goals in practice: Rehabilitation Plans A
- 13.C4 Goals in practice: Rehabilitation Plans B
- PART D:
POST-TEST
AND RESOUCES - 13.D1 Resources
- 13.D2 Take
the POST-Test
13.B2 Team processes and goal setting
- (i)
Putting
it all
together - (ii)
Team
processes
& goal setting - (iii)
Teams
Process
- (iv)
Sample
Team
Guidelines - (v)
Goal setting
&individual
workers - (vi)
Individual
processes
Developing Team Processes to Facilitate High Quality Goal Setting
This training provides individuals with skills and knowledge in writing SMART goals and how they can be used to support client centred practice in rehabilitation.
However, to implement these skills, the whole team you work with may need to be aware of these skills and be involved in negotiating what changes may be needed to current processes.
While this is beyond the scope of this training, we have provided some information to help you consider what may be required in the context or service in which you work.
What this section aims to do is provide some suggestions for the elements of processes to facilitate high-quality goal-setting.
The specific processes that best facilitate high-quality goal setting within each setting will vary, as these will be influenced by internal policies and practices.
Clinicians and teams can use this section to revise or develop their own processes, if desired. Changing processes to improve goal-setting is a worthwhile quality improvement project as effective goals can be used to motivate clients, guide clinical practice and evaluate client and service outcomes (e.g. monitor the number of participation level goals that are achieved; audit level of client engagement in goal setting).
To what extent does your team
Print your responses for your records
What needs to happen in your service to improve practice?
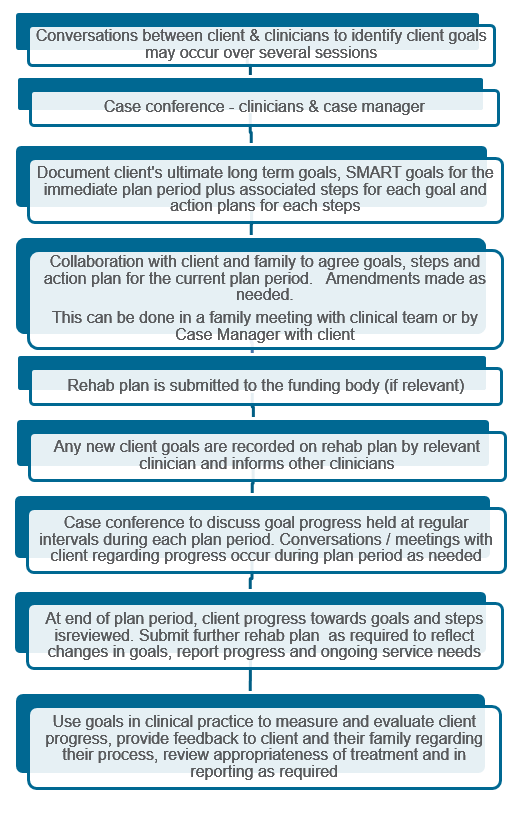
Goal Setting Processes within Rehabilitation Units / Teams
This TAB describes an example of an interdisciplinary, client centred goal setting process that would suit a team of clinicians who primarily work together in a single service.
The aim is to provide structure to conversations and meetings that frequently occur and to ensure that client priorities drive the development of a cohesive rehabilitation plan. It is easier to write high quality, participation level client centred goals when an interdisciplinary approach is used. The order and elements may need to be adjusted to suit different environments and services.
The key features of an interdisciplinary goal setting process include:
All clinicians discuss goals with the client, although one person may take the lead
The client’s goals direct the action plan
More than one meeting with the client may be needed to identify their goal – dependent on client age, nature and severity of injury and adjustment to injury
Clinicians complete necessary assessments to inform the development of an action plan and to provide an understanding of the client’s current level of functioning and needs
Team meetings or case conferences are needed to review client goals and assessment results as well as develop an action plan. The client’s long term goals and SMART rehabilitation goals and steps need to be defined and reported. Team meetings / case conferences are required regularly to support ongoing rehabilitation planning and reporting
Clients can be engaged in determining and agreeing to goals, steps and action plans in collaboration with clinicians throughout their rehabilitation program. Accommodating client preferences is consistent with current definitions of evidence based practice
The process is cyclical – steps are repeated as the client makes progress and new goals are set
New goals may be identified during plan periods and these need to be communicated to all involved. This can be done via email or a further meeting may be needed.
An example of how these principles can inform a team, process is outlined in in next TAB.
Team Process
Sample Team Guidelines
[Service] Procedure
- Within [one to two weeks] of admission to the [service] a rehabilitation planning and initial goal setting session will be scheduled by [who].
- Representatives from all areas of the multidisciplinary team are expected to prioritise attendance at this session.
- The rehabilitation planning session sheet (see appendix 1) is to be completed by the team as a collective, outlining the person’s previous roles, responsibilities, routines and interests and early identification of potential barriers to the rehabilitation process are to be recorded (e.g. poor accessibility for wheelchair within the home, limited social supports). The anticipated goal pathway (see section below) should be determined by the team.
- A key worker is designated within the treating team.
Rehabilitation planning and initial goal setting session
Key worker responsibilities
The keyworker is designated at the time of the rehabilitation planning sessions. The key worker’s responsibilities include:
- Chairing and documentation of goal setting sessions
- Providing leadership to the team during the rehabilitation planning session.
- Leading and facilitating team conversations with the client and/or their family during goal setting sessions including identifying goals and providing feedback on goal attainment.
- Ensuring that all team members contribute to the development of goal action plans and that these are filed in the person’s clinical record.
- Ensuring that goal setting sessions and staff attendance are documented in the person’s clinical record.
- Liaising with the Inpatient Program Coordinator on the frequency of goal setting sessions required and advising on when goals are due to be reviewed.
- Providing feedback to the treating staff specialist on current goals and goal attainment including within case conference.
- Acting as a key point of contact for communication between the client, their family and the multidisciplinary team.
A staff member can only be designated as a key worker once they have under taken the Goal Training, either with a service Goal Setting trainer or attendance at an external training course.
Goal setting sessions
Identifying what will be recorded as the person’s goals from the following circumstances
Person generated goal: The goal is identified by the person themselves as their priority. The goal will be recorded in the person’s words. It may also be restated to maximise the potential for measurement of the goal, but it directly relates to the anticipated level of change desired by the individual.
Person focused goal with family assistance: The goal relates to how the person will benefit from therapy but may not be an explicit priority identified by that person. The person may not be able to identify the link between shorter term goals and their ultimate goal. This may be influenced by their level of insight, adjustment to their disability and time since injury. For example, a person may express that their goal is to return home. A person focused goal may be that the person will be able to spend the weekend at home with their family by the end of the month, as a step towards their ultimate goal of being able to return home.
The person is unable to generate their own goal however their family are able to clearly articulate what they believe would be the person’s priorities/in their best interest. For example, a person who is in a minimally conscious state is unable to consistently use a form of communication to express their wants/goals. Sometimes it may include the family eg. Jean’s mum will wheel her into the garden and sit with her for 30 mins.
Processes
- During the goal planning session, all members of the treating multidisciplinary team attend to the person at their bedside or meet with family member depending on the goal pathway. The key worker is responsible for facilitating discussion with the client/family, including their current progress, barriers and using motivational interviewing techniques to assist the client/family in generating their goal.
- Once the goal has been determined and a timeframe set, the goal is to be written or typed on the goal sheet and displayed in the client’s room (and a copy placed in the goals section of their clinical record).
- Once the client’s goal and goal pathway have been determined, a goal action plan must be completed with contributions from all members of the multidisciplinary team, outlining the actions that will be taken to facilitate the client achieving their goal.
- At the subsequent goal planning session, the goal action plan will be reviewed and scored for goal attainment.
- Feedback on goal attainment is provided to the client and/or their family by the key worker with the multidisciplinary team. A new goal and new goal action plan are then established.
- Feedback on goal action plans and client progress is provided by the key worker to the multidisciplinary team during case conference, with additional contributions on progress provided by members of the treating team as needed
- The key worker will also provide additional feedback directly to the treating specialist following all goal planning sessions on the client’s progress and goal action plan.
- The frequency of goal planning sessions will be dependent on the needs of the individual client and their goal and can occur weekly, fortnightly or monthly.
- The key worker is responsible for informing the Program Coordinator at the end of each goal planning session as to when the goals are due to be reviewed.
Key attributes necessary for procedural compliance:
- Knowledge of processes
- Skills to implement processes to the standard required
NOTE: The Liverpool Brain Injury Rehabilitation Unit is acknowledged for their work on these guidelines
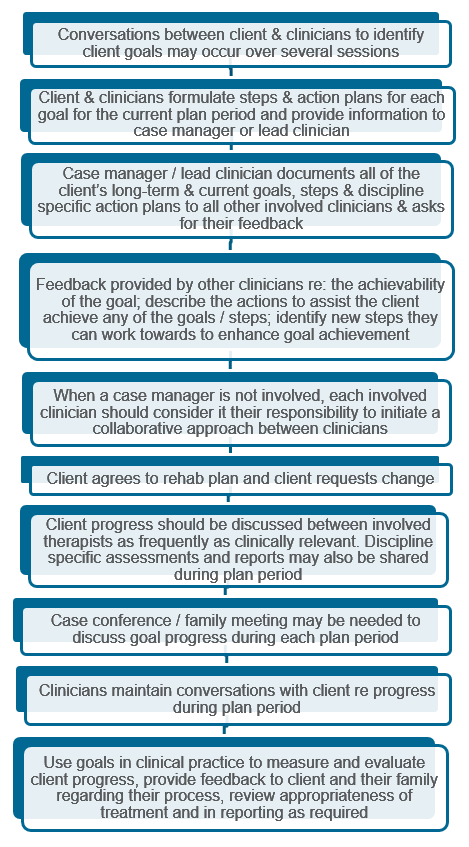
Goal Setting Processes for Single Discipline / Sole Workers
It can be harder to negotiate a ‘team’ based approach when you work as a sole provider or discipline working with clinicians from different services to meet the needs of clients.
There tends to be less face to face meetings with all the clinicians involved.
The process is very similar to that for those in rehabilitation units / teams but the information obtained in the case conference may be completed over time and managed without a face to face meeting.
The key features include:
- All clinicians have conversations with the client about the client’s goals. They need to communicate information about the client’s preferences to the lead clinician
- The lead clinician needs to collaborate with the client and clinicians to agree the goals, steps and action plan for the plan period
- The lead clinician should document the client’s long-term and current goals, the therapy-specific steps and action plans that have been agreed to by all clinicians and seek feedback regarding whether they:
- have any comment to make about the achievability of the goal from their particular professional perspective
- consider that they need to play a role towards any of the goals. If they do, request that they share with you their steps and action plans and the degree to which the client is aware of these
- Progress should be discussed between involved therapists as frequently as seems clinically relevant
- The lead clinician completes the rehabilitation plan to cover services required by all providers. Additional discipline specific reports may be needed to support the rehabilitation plan. Progress from each discipline should be provided in relation to the identified goals and steps
- When a lead clinician is not involved, each involved clinician should consider it their responsibility to initiate and maintain a collaborative approach between clinicians to ensure client centred practice.
On the next TAB is an example of a goal setting process for single discipline clinicians / sole workers For further information about a collaborative interdisciplinary approach to client centred participation level goals, see NSW Health’s Rehabilitation Redesign Project Model of Care.
Individual process