- SELF STUDY MODULES
- 1. Intro to TBI
- 2. Communication
- 3. Skills for independence
- 4. Cognitive changes
- 5. Behaviour changes
- 6. Sexuality
- 7. Case management (BIR)
- 8. No longer available
- 9. Mobility & motor control
- 10. Mental health & TBI:
an introduction - 11. Mental health problems
and TBI: diagnosis
& management - 12. Working with Families
after Traumatic Injury:
An Introduction - 13. Goal setting
- 13.0 Aims
- 13.0A Take the PRE-Test
- PART A:
SETTING GOALS
IN REHABILITATION
- PART B: TEAMS &
GOALS - 13.B1 Collaborative goal setting
- 13.B2 Rehabilitation teams & goals
- 13.B3 Quality & Evaluation checklists
- 13.B4 Take home messages
- PART C: WORKSHEETS
- 13.C1 SMARTAAR
Goals Worksheet A - 13.C2 SMARTAAR
Goals Worksheet B - 13.C3 Goals in practice: Rehabilitation Plans A
- 13.C4 Goals in practice: Rehabilitation Plans B
- PART D:
POST-TEST
AND RESOUCES - 13.D1 Resources
- 13.D2 Take
the POST-Test
13.B1 Collaborative goal setting
- (i) Approaches to
goal setting - (ii) Collaboration
- (iii) Understanding collaborative
goal setting - (iv) Test your
knowledge
Approaches to Rehabilitation that Influence Goal Setting
Three different styles or models of teamwork are typically used.
- Multidisciplinary
- Interdisciplinary
- Transdisciplinary
There is a tendency to use team terminology somewhat interchangeably, but there are important differences between “multidisciplinary” and “interdisciplinary”.
While the multidisciplinary team evolved from the medical model, utilizing the clinical expertise of each discipline, the interdisciplinary team emphasizes an integrated approach to care planning.
Other team models that have been proposed in other domains (including mental health and early intervention community health) incorporate a trans-disciplinary model where there each team member becomes sufficiently familiar with the roles and approaches of other team members as to blur the disciplinary boundaries and enable the team to focus on the problem.
From a team perspective, there are three approaches to goal setting in the rehabilitation
setting:
Multidisciplinary
Multidisciplinary, in which each different clinical discipline sets discipline
specific goals without collaboration with other therapists
- Clinicians work independently, but recognize and value contributions of other team members.
- The role of each team member is strictly defined.
- Clinicians provide separate evaluations,
- Clinicians set goals that are specific to their discipline and implement individual intervention plans.
- Team members meet to exchange information
Disadvantages:
- Disciplinary silos impede efforts toward collaboration.
- Individual therapies not taking into account other influences on performance
Interdisciplinary
Interdisciplinary, in which a group of health professionals from different
disciplines work towards common goals that are set in collaboration, including
client involvement in the goal setting
- Collaboration is required among team members for the evaluation, assessment, and development of the intervention plan.
- All clinicians are working towards the common goal.
- Clinicians can utilize knowledge and expertise from other team members to add value to their own approach
Disadvantages:
- Professional boundaries may become blurred and it may be perceived that there is questioning of professional judgment.
Transdisciplinary
Transdisciplinary, in which one team member acts as the primary therapist with
other therapists providing information and advice.
- Team members provide joint evaluations and work together to develop goals and carry out interventions.
- One team member will then usually be the individual that the family interacts with, and they will provide all the intervention although they may consult with other clinicians
Disadvantages:
- Disciplinary lines are blurred
- Team members share role functions to a high degree
- Reduction of specialisation
An interdisciplinary collaborative approach is best practice in brain injury rehabilitation
An interdisciplinary collaborative approach to rehabilitation and goal setting is recognised as best practice in brin injury rehabilitation
Using an interdisciplinary collaborative approach has the following benefits:
-
it facilitates a focus on participation-level goals
-
it emphasises the involvement of the client in goal-setting
-
it facilitates an efficient approach to goal-achievement by ensuring that necessary input from multiple disciplines is provided concurrently, without duplication of roles.
Collaborative goal setting
Collaborative goal setting is an essential and central part of an interdisciplinary process
and is considered best practice in brain injury rehabilitation.
The benefits include:
a) an emphasis on the involvement of the client in goal setting:
o not including the client in the goal setting process increases their dependence on the therapist, which is contrary to the purpose of rehabilitation
o a positive relationship between the level of client involvement in goal setting and rehabilitation outcomes has been demonstrated
o non-collaboration with the client in regards to goal setting has been cited as a reason for neuro-rehabilitation failureb) prevention of the duplication of roles
c) facilitation of a focus on participation level goals, which are recognised as best practice in rehabilitation
Understanding collaborative goal setting
While the overarching approach to rehabilitation may be influenced by service and organisational drivers, clinicians are encouraged to facilitate a collaborative approach to goal setting as much as possible.
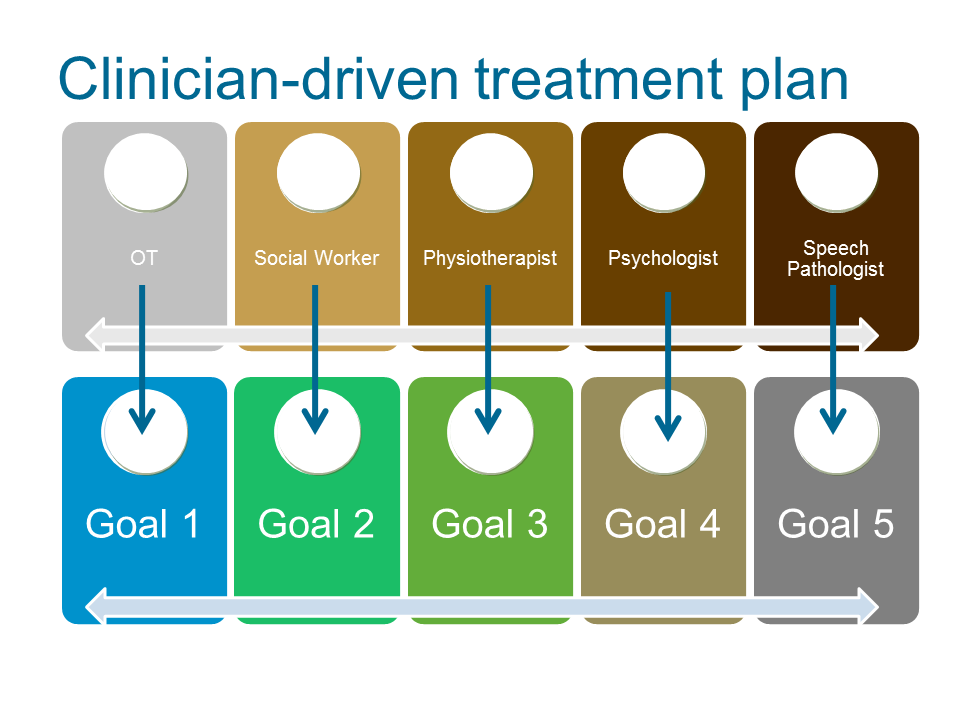
This differs from a more traditional approach clinicians drive the treatment plan. Team and client communication is directed by discipline specific goals and interventions.
Interdisciplinary collaborative approach
Using an interdisciplinary collaborative approach, client goals direct the action plan rather than individual disciplines identifying goals for the client specific to their role.
Communication is structured around the client’s rehabilitation goals and each discipline identifies if and how they can contribute to each goal, e.g. Instead of discussing OT goals, the OT will ask, does the client have any goals that require OT input? Figure 7 compares the impact of client goal and clinician driven treatment plans on team collaboration and roles.
A collaborative approach that enables the client goals to drive the treatment plan is particularly important when the client identifies participation level goals. Participation-level goals can be more complex and often require the input of several disciplines concurrently.
Input from multiple therapists is often required from the beginning to ensure a participation-level goal is realistic.
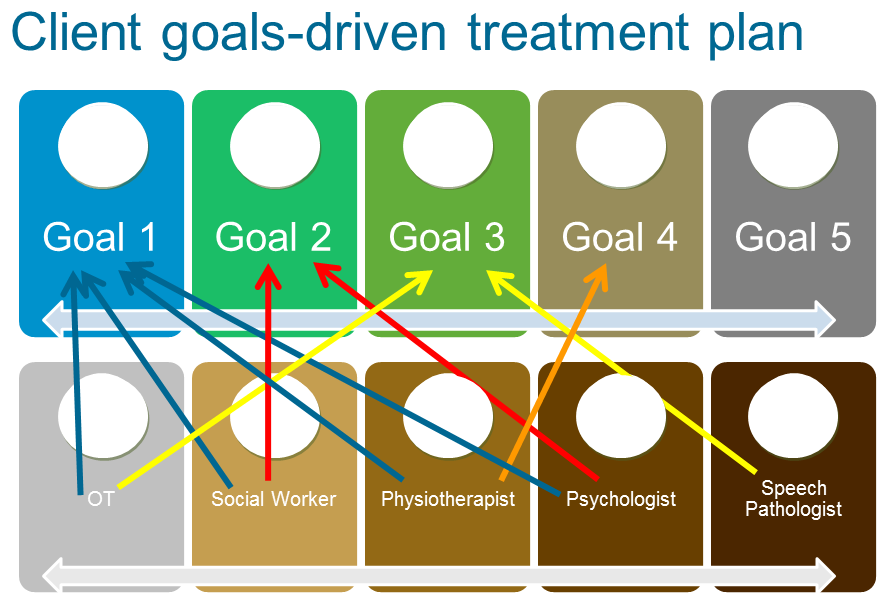
For example, a client whose goal is to return to work following multi-trauma from a car accident may realistically have the physical ability to do so within three months, but not the psychological well-being. If there is no liaison between the physiotherapist and psychologist, it is possible that the physiotherapist may be setting the client up to fail.
It is largely because of the importance of participation-level goals that an interdisciplinary approach is considered best practice (see Figure 8).
The impact of introducing a more interdisciplinary collaborative approach on time demands will depend on the current approach to service delivery and how meetings and communication about clients are organised. A common response to the suggestion that goal setting be a collaborative approach is client meetings already take too long and that this will take even more time. Discussions about goals should not be separate to other discussions about clients. All discussions about clients should be relevant to their goals and how these are going to be achieved. Goals offer structure and focus to the client discussions that are already occurring.
Within a multidisciplinary unit, changing to a collaborative goal setting approach does not always increase the time demands, but can make meetings and reporting more streamlined.
Rather than case conference meetings being structured by headings of each discipline involved – so that that each therapist speaks once to provide feedback regarding progress in their sessions - it is more useful to structure case conferences by headings of the client’s goals, with each therapist then reporting on progress and outstanding needs relevant to that goal. This ensures that all are aware of the current goals being worked towards and provides the opportunity for each therapist to provide any input relevant to that goal that other therapists may not have considered. In some settings additional meetings with clients may be needed. In others the focus of existing contact with client and clinicians is more goal directed but able to be implemented within current schedules.
The suggestion that case conferences be structured in terms of current goals is sometimes met with comments that this structure is too restrictive and doesn’t allow for important information that doesn’t relate to a goal to be discussed. Everything that is discussed in a formal case conference should relate to a client’s goal. If it doesn’t, it is very likely that there is a goal that has not been formally identified. This is often a big change from how people are used to working.
A collaborative goal setting approach is not confined to use within multidisciplinary health units. It is just as relevant when the client is receiving care from multiple private providers.
Regular joint meetings may not always be practical, but all health professionals involved should be aware of the client’s goals and everyone’s role in assisting the achievement of these. When individual clinicians work collaboratively with others, increased time may be required - this requirement can be discussed with the funder. Further information on this point is provided in Section 0.
Test your knowledge
1. Participation level goals are considered best practice in rehabilitation.
2. All clients can identify all their own rehabilitation goals
3. Input from multiple therapists is often required from the beginning to ensure a participation-level goal is realistic.
4. A collaborative goal setting approach is not confined to use within multidisciplinary health units. It is just as relevant when the client is receiving care from multiple private providers.
5. Using an interdisciplinary collaborative approach, client goals direct the action plan rather than individual disciplines identifying goals for the client specific to their role.
6. While participation-level goals are advocated as best practice, and are most likely to reflect the longer term priorities of clients, at times impairment goals can also be appropriate.
7. Non-collaboration with the client in regards to goal setting has been cited as a reason for neuro-rehabilitation failure
8. A collaborative approach to goal-achievement by ensuring that necessary input from multiple disciplines is provided concurrently is less efficient than a non-collaborative approach.