- SELF STUDY MODULES
- 1. Intro to TBI
- 2. Communication
- 3. Skills for independence
- 4. Cognitive changes
- 5. Behaviour changes
- 6. Sexuality
- 7. Case management (BIR)
- 8. No longer available
- 9. Mobility & motor control
- 10. Mental health & TBI:
an introduction - 11. Mental health problems
and TBI: diagnosis
& management - 12. Working with Families
after Traumatic Injury:
An Introduction - 13. Goal setting
5.5 Understanding anger
- i) Intro
- ii) Potential
triggers - iii) Early
warning signs - iv) Emotional
model - v) Recognise
your feelings - vi) Strategies
i) Introduction
Anger management problems can stem from the brain injury itself, as well as from problems with reduced self-control, impulsivity and lowered frustration tolerance. It is important to be able to:
- a) identify potential triggers of anger
- b) identify 'early warning signals’
- c) understand an emotional model of anger
- d) recognise your feelings and
- e) have strategies for managing clients who display anger.
ii) Potential triggers of anger following a TBI
Potential triggers of anger following a TBI include the following:
- Lack of Sleep
- Pain/headaches
- Noise sensitivity
- Changed self image
- Feeling angry about accident or injury
- Worries about future/finances
- Coping with change
- Lack of understanding from others (friends/family/medical professionals etc)
- Frustration (personal and/or sexual)
- Feeling out of control when organising daily life due to numerous medical/legal appointments
- Personality clashes/changes to relationships and social activities
iii) Early warning signals
As a person becomes angry, changes occur at a physical, emotional and/or cognitive level. If these changes are caught early enough (i.e. before a person loses their temper) then they can be used as an ‘early warning system’.
The following changes are often used as guideposts to alert a person that they are becoming angry.
Physical |
Emotional |
Cognitive |
Muscle tension Temperature change Tremor/shaking Sweating Heart pounding Clenched fists |
Irritated Frustrated Moody Unsettled Feeling upset |
Changes to thoughts include: Racing Jumbled Irrational Jumping to conclusions |
iv) Principles of anger
To better understand how to manage anger it is useful to understand the principles of anger that include:
- a scale of anger - for example calm (no anger) to aggressive.
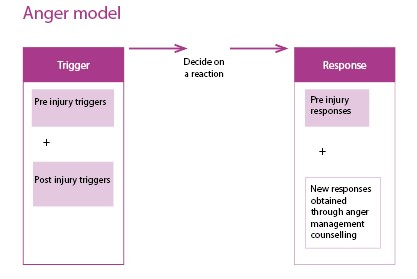
- an anger model showing triggers and responses
- recognition that anger can be a secondary feeling
Scale of anger
Anger escalates in intensity if it is not monitored or managed. A calm person can become angry and then aggressive, if triggered.
(18 sec)
Triggers and responses
In thinking about how people with TBI can change from being calm to being angry or aggressive it is useful to think about triggers and responses (both pre-injury and post-injury).
Anger as a secondary feeling
Anger can be a secondary feeling and so it is important to ask the question: was there a primary feeling?
v) Recognising your Feelings
Remember that the behaviour is not necessarily directed at you.
Why is the person angry with you?
Proximity
What are you feeling?
It is important to recognise and identify your feelings.
What to do in relation to your feelings?
- Accept your own feelings about the situation
- Talk to family, staff & friends and discuss how you are feeling
- Recognise that you are only human and that you can also be affected by stress, frustration and anger
- Use stress and anger management strategies yourself
vi) Strategies for staff managing clients who display anger
In any difficult situation it is important to maintain focus on the problem not the behaviour.
You can achieve this by:
- Remaining calm
- Walking away/removing yourself from situation temporarily (if safe/appropriate to do so) to regain composure
- Use non-threatening/relaxed body language and tone
- Take slow deep breaths/use a deep breathing technique
- Discontinue a conversation/discussion that is eliciting a negative emotional reaction in you or the client
- Avoid compounding the problem with the use of alcohol or drugs to ‘cope’
- Requesting a break from the client (either permanently or temporarily)